Staffing Mandates in the Midst of COVID
The long-term care industry is no stranger to workforce shortages. Workforce recruitment and retention are two challenges that have been persistent for years. Now, add a pandemic.
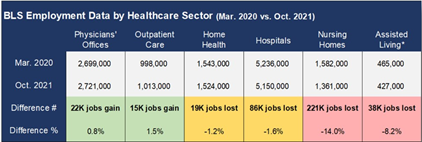
According to the Bureau of Labor Statistics, nursing homes alone have seen their industry’s employment level drop by 14 percent or 221,000 jobs since the beginning of the pandemic.
 The American Health Care Association and National Center for Assisted Living (AHCA/NCAL) released results from their “State of the Long Term Care Industry” survey of nursing home and assisted living providers – here are a few highlights:
The American Health Care Association and National Center for Assisted Living (AHCA/NCAL) released results from their “State of the Long Term Care Industry” survey of nursing home and assisted living providers – here are a few highlights:
- 86% of nursing homes and 77% of assisted living providers said their workforce situation has gotten worse in recent months
- 58% of nursing homes are limiting new admissions
- 78% of nursing homes and 61% of assisted living communities are concerned workforce challenges might force them to close
The staffing situation became so urgent in 2021 that the New York National Guard sent Army medics and Air Force medical technicians to nursing homes across the state in December.
And now, with the new year comes yet another staffing challenge for those of us in the long-term care industry in New York – keeping up with the new staffing mandate. As of January 1, 2022 the minimum nurse staffing regulation dictates the number of hours of care that must be provided by certified nurse aides, registered professional nurses, and licensed practical nurses.
Before I get into the details, I want to explicitly state that I believe the one thing many of us have in common is that we want to see our long-term care residents thriving. That looks different for each and every individual. My personal preference is to look at the data we have and the residents we serve and make decisions based on those two factors.
What does that data show? Here’s what we know about the relationship between staffing and quality of care according to the CMS Nursing Home Compare data:
- Of the 377 homes receiving 3 or fewer stars for staffing, 75.6%, were awarded 4 or 5 stars for quality measures that indicate positive outcomes
- Conversely, 241 homes received 4 or 5 stars for staffing, yet 63.5% percent, scored 3 or fewer stars on their survey (periodic inspection).
The individuals mentioned in the staffing mandate indeed provide essential care to our residents at Loretto – but so do our therapy personnel, activities aides, housekeeping staff, and more. All of them are notably absent from this staffing mandate.
At Loretto, our focus is on acuity-based care. In other words, much like my desire to get to know employees at Loretto, I also want all of us to get to know our residents. Once we get to know them, my goal is to tailor their care to their needs. Our residents do not have the one-size-fits-all care that the minimum staffing mandate assumes. Some of them may have a higher clinical need and require more hours from an RN; others may have a lower clinical need but benefit from more programming our activities team can offer them.
But how can you be assured that Loretto, and other long term care facilities are providing an adequate number of appropriate staff? Here are a couple of ways we are already being held accountable:
- CMS uses staffing in the Nursing Home Compare 5-star rating system provided to the public (staffing rating is based on total nursing hours per resident and RN hours per resident per day).
- New York’s Nursing Home Quality Pool includes both the CMS 5-star staffing rating and the level of temporary contract/agency staff.
LeadingAge New York estimates that the typical downstate nursing home will see an increase of $15 per resident per day to accommodate the increase in staffing to meet this mandate. For a home serving 200 residents, that’s over $1 million per year for increased aide staffing. That’s assuming the nursing home can find, recruit and retain the nurses and aides to hire. While nursing is a rapidly growing field, some schools can only admit a small number of their applicant pool because universities are dealing with their own cuts in funding and loss of staff positions and can’t support the educational needs of a larger number of nursing students.
There’s no doubt this is a complex issue. My purpose in this blog post is to share my personal point of view – one shared by many in the long-term care industry. So what is the solution? LeadingAge New York sums it up in a way I couldn’t have said better myself:
“Before mandating a number, the State should be looking at ways to encourage entrance into the field, promote recruitment and retention of nurses and aides, assist nursing education programs that are struggling, assisting (as they have in the past) with the cost of nursing education, reducing burdensome paperwork requirements that take direct care workers away from the bedside, and promoting the field of nursing in general.”

